Treatment And Cause
Overview
Over 60 Million Americans suffer from Adult Acquired Flatfoot (AAF), otherwise known as Posterior Tibial Tendon Dysfunction or PTTD. This condition generally occurs in adults from 40-65 years of age, and it usually only occurs in one foot, not both. The Posterior Tibial (PT) Tendon courses along the inside part of the ankle and underneath the arch of the foot. It is the major supporting structure for the arch. Over time, the tendon becomes diseased, from overuse, and starts to lose it's strength. As a result, the arch begins to collapse, placing further strain on the PT Tendon, leading to further decrease in tendon strength, which causes further collapse of the arch. This is described as a progressive deformity because it will generally get worse over time. 
Causes
As discussed above, many different problems can create a painful flatfoot. Damage to the posterior tibial tendon is the most common cause of AAFD. The posterior tibial tendon is one of the most important tendons of the leg. It starts at a muscle in the calf, travels down the inside of the lower leg and attaches to the bones on the inside of the foot. The main function of this tendon is to support the arch of your foot when you walk. If the tendon becomes inflamed or torn, the arch will slowly collapse. Women and people over 40 are more likely to develop problems with the posterior tibial tendon. Other risk factors include obesity, diabetes, and hypertension. Having flat feet since childhood increases the risk of developing a tear in the posterior tibial tendon. In addition, people who are involved in high impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Inflammatory arthritis, such as rheumatoid arthritis, can cause a painful flatfoot. This type of arthritis attacks not only the cartilage in the joints, but also the ligaments that support the foot. Inflammatory arthritis not only causes pain, but also causes the foot to change shape and become flat. The arthritis can affect the back of the foot or the middle of foot, both of which can result in a fallen arch. An injury to the tendons or ligaments in the foot can cause the joints to fall out of alignment. The ligaments support the bones and prevent them from moving. If the ligaments are torn, the foot will become flat and painful. This more commonly occurs in the middle of the foot (Lisfranc injury), but can also occur in the back of the foot. Injuries to tendons of the foot can occur either in one instance (traumatically) or with repeated use over time (overuse injury). Regardless of the cause, if tendon function is altered, the forces that are transmitted across joints in the foot are changed and this can lead to increased stress on joint cartilage and ligaments. In addition to tendon and ligament injuries, fractures and dislocations of the bones in the midfoot can also lead to a flatfoot deformity. People with diabetes or with nerve problems that limits normal feeling in the feet, can have collapse of the arch or of the entire foot. This type of arch collapse is typically more severe than that seen in patients with normal feeling in their feet. In addition to the ligaments not holding the bones in place, the bones themselves can sometimes fracture and disintegrate without the patient feeling any pain. This may result in a severely deformed foot that is very challenging to correct with surgery. Special shoes or braces are the best method for dealing with this problem.
Symptoms
Symptoms shift around a bit, depending on what stage of PTTD you?re in. For instance, you?re likely to start off with tendonitis, or inflammation of the posterior tibial tendon. This will make the area around the inside of your ankle and possibly into your arch swollen, reddened, warm to the touch, and painful. Inflammation may actually last throughout the stages of PTTD. The ankle will also begin to roll towards the inside of the foot (pronate), your heel may tilt, and you may experience some pain in your leg (e.g. shin splints). As the condition progresses, the toes and foot begin to turn outward, so that when you look at your foot from the back (or have a friend look for you, because-hey-that can be kind of a difficult maneuver to pull off) more toes than usual will be visible on the outside (i.e. the side with the pinky toe). At this stage, the foot?s still going to be flexible, although it will likely have flattened somewhat due to the lack of support from the posterior tibial tendon. You may also find it difficult to stand on your toes. Finally, you may reach a stage in which your feet are inflexibly flat. At this point, you may experience pain below your ankle on the outside of your foot, and you might even develop arthritis in the ankle.
Diagnosis
Clinicians need to recognize the early stage of this syndrome which includes pain, swelling, tendonitis and disability. The musculoskeletal portion of the clinical exam can help determine the stage of the disease. It is important to palpate the posterior tibial tendon and test its muscle strength. This is tested by asking patient to plantarflex and invert the foot. Joint range of motion is should be assessed as well. Stiffness of the joints may indicate longstanding disease causing a rigid deformity. A weightbearing examination should be performed as well. A complete absence of the medial longitudinal arch is often seen. In later stages the head of the talus bone projects outward to the point of a large "lump" in the arch. Observing the patient's feet from behind shows a significant valgus rotation of the heel. From behind, the "too many toes" sign may be seen as well. This is when there is abducution of the forefoot in the transverse plane allowing the toes to be seen from behind. Dysfunction of the posterior tibial tendon can be assessed by asking the patient to stand on his/her toes on the affected foot. If they are unable to, this indicates the disease is in a more advanced stage with the tendon possibly completely ruptured.
Non surgical Treatment
Flatfoot deformity can be treated conservatively or with surgical intervention depending on the severity of the condition. When people notice their arches flattening, they should immediately avoid non-supportive shoes such as flip-flops, sandals or thin-soled tennis shoes. Theses shoes will only worsen the flatfoot deformity and exacerbate arch pain. Next, custom orthotics are essential for people with collapsed arches. Over-the-counter insoles only provide cushion and padding to the arch, whereas custom orthotics are fabricated to specifically fit the patient?s foot and provide support in the arch where the posterior tibial tendon is unable to anymore. Use of custom orthotics in the early phases of flatfoot or PTTD can prevent worsening of symptoms and prevent further attenuation or injury to the posterior tibial tendon. In more severe cases of flatfoot deformity an ankle foot orthosis (AFO) such as a Ritchie brace is needed. This brace provides more support to the arch and hindfoot rather than an orthotic but can be bulky in normal shoegear. Additional treatment along with use of custom orthotics is use of non-steroidal anti-inflammatories (NSAIDS) such as Advil, Motrin, or Ibuprofen which can decrease inflammation to the posterior tibial tendon. If pain is severe, the patient may need to be placed in a below the knee air walker boot for several weeks which will allow the tendon to rest and heal, especially if a posterior tibial tendon tear is noted on MRI. 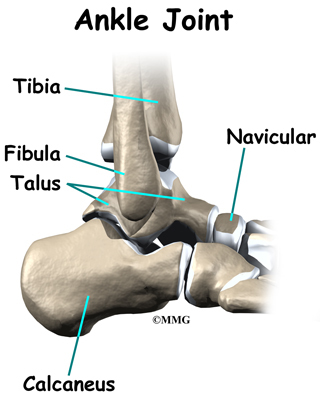
Surgical Treatment
Flatfoot reconstruction (osteotomy). This is often recommended for flexible flatfoot condition. Flatfoot reconstruction involves cutting and shifting the heel bone into a more neutral position, transferring the tendon used to flex the lesser toes (all but the big toe) to strengthen the posterior tibial tendon, and lengthening the calf muscle. Fusion (also known as triple arthrodesis). Fusion involves fusing, or making stiff, three joints in the back of the foot the subtalar, talonavicular, and calcaneocuboid joints, to realign the foot and give it a more natural shape. Pins or screws hold the area in place until it heals. Fusion is often recommended for a rigid flatfoot deformity or evidence of arthritis. Both of these surgeries can provide excellent pain relief and correction.
Achilles Tendon Rupture Long Leg Cast Removal
Overview  The Achilles tendon is the thickest and strongest tendon in the human body. It plays a very important role in most sport activities and is particularly vulnerable to overloading from repetitive running and jumping. The Achilles tendon forms a joint distal tendon for the gastrocnemius and the soleus muscles. These muscles combine to form the triceps surae muscle. Athletes who sustain Achilles tendon ruptures most frequently are those who participate in ball sports that demand rapid changes of direction and quick, reactive jumps (e.g., tennis, squash, badminton, and soccer), in addition to runners and jumpers in track and field. Sometimes a patient with a ruptured tendon has a history of long-term pain localized to the tendon, but more often the rupture occurs without warning. Such ruptures are often caused by degenerative changes in the tendon (tendinosis), usually in the segment of the tendon that has the worst blood supply. This segment extends from 2 to 6 cm proximal to the insertion of the tendon onto the calcaneus. Causes Often an Achilles rupture can occur spontaneously without any prodromal symptoms. Unfortunately the first "pop" or "snap" that you experience is your Achilles tendon rupture. Achilles tendon rupture most commonly occurs in the middle-aged male athlete (the weekend warrior who is engaging in a pickup game of basketball, for example). Injury often occurs during recreational sports that require bursts of jumping, pivoting, and running. Most often these are tennis, racquetball, squash, basketball, soccer, softball and badminton. Achilles rupture can happen in the following situations. You make a forceful push-off with your foot while your knee is straightened by the powerful thigh muscles. One example might be starting a foot race or jumping. You suddenly trip or stumble, and your foot is thrust in front to break a fall, forcefully over stretching the tendon. You fall from a significant height. It does appear that previous history of Achilles tendonitis results in a degenerative tendon, which can grow weak and thin with age and lack of use. Then it becomes prone to injury or rupture. Certain illnesses (such as arthritis and diabetes) and medications (such as corticosteroids and some antibiotics) can also increase the risk of rupture. Symptoms Symptoms of an Achilles tendon rupture usually directly follow a traumatic event where the foot is forced in an upward position at the ankle, causing a sudden tight stretch of the Achilles tendon. There can also be a direct blow to the tendon causing a rupture. There is typically a popping feeling or even a popping sound described during the occurance of the rupture. Typically there is pain with swelling in the region. Often the patient is unable to put weight on this foot as there is too much pain. Diagnosis If an Achilles tendon rupture is suspected, it is important to consult a doctor straight away so that an accurate diagnosis can be made and appropriate treatment recommended. Until a doctor can be consulted it is important to let the foot hang down with the toes pointed to the ground. This prevents the ends of the ruptured tendon pulling any farther apart. The doctor will take a full medical history, including any previous Achilles tendon injuries and what activity was being undertaken at the time the present injury occurred. The doctor will also conduct a physical examination and will check for swelling, tenderness and range of movement in the lower leg and foot. A noticeable gap may be able to be felt in the tendon at the site of the rupture. This is most obvious just after the rupture has occurred and swelling will eventually make this gap difficult to feel. One test commonly used to confirm an Achilles tendon rupture is the Thomson test. For this test the patient lies face down on an examination table. The doctor then squeezes the calf muscles; an action that would normally cause the foot to point like a ballerina (plantar flexion). When a partial rupture has occurred the foot's ability to point may be decreased. When a complete rupture has occurred, the foot may not point at all. Ultrasound scanning of the Achilles tendon may also be recommended in order to assist with the diagnosis. Non Surgical Treatment Once the Achilles tendon is partially damaged, one should exercise great care. The risk of rupture is high and if pain is associated with walking, one should consult with an orthopedic surgeon or a sports physician. A complete rupture of the Achilles tendon is never treated at home. It is important to understand that there are no minerals, nutrients, or herbs to treat Achilles tendon injury and any delay just worsens the recovery.
The Achilles tendon is the thickest and strongest tendon in the human body. It plays a very important role in most sport activities and is particularly vulnerable to overloading from repetitive running and jumping. The Achilles tendon forms a joint distal tendon for the gastrocnemius and the soleus muscles. These muscles combine to form the triceps surae muscle. Athletes who sustain Achilles tendon ruptures most frequently are those who participate in ball sports that demand rapid changes of direction and quick, reactive jumps (e.g., tennis, squash, badminton, and soccer), in addition to runners and jumpers in track and field. Sometimes a patient with a ruptured tendon has a history of long-term pain localized to the tendon, but more often the rupture occurs without warning. Such ruptures are often caused by degenerative changes in the tendon (tendinosis), usually in the segment of the tendon that has the worst blood supply. This segment extends from 2 to 6 cm proximal to the insertion of the tendon onto the calcaneus. Causes Often an Achilles rupture can occur spontaneously without any prodromal symptoms. Unfortunately the first "pop" or "snap" that you experience is your Achilles tendon rupture. Achilles tendon rupture most commonly occurs in the middle-aged male athlete (the weekend warrior who is engaging in a pickup game of basketball, for example). Injury often occurs during recreational sports that require bursts of jumping, pivoting, and running. Most often these are tennis, racquetball, squash, basketball, soccer, softball and badminton. Achilles rupture can happen in the following situations. You make a forceful push-off with your foot while your knee is straightened by the powerful thigh muscles. One example might be starting a foot race or jumping. You suddenly trip or stumble, and your foot is thrust in front to break a fall, forcefully over stretching the tendon. You fall from a significant height. It does appear that previous history of Achilles tendonitis results in a degenerative tendon, which can grow weak and thin with age and lack of use. Then it becomes prone to injury or rupture. Certain illnesses (such as arthritis and diabetes) and medications (such as corticosteroids and some antibiotics) can also increase the risk of rupture. Symptoms Symptoms of an Achilles tendon rupture usually directly follow a traumatic event where the foot is forced in an upward position at the ankle, causing a sudden tight stretch of the Achilles tendon. There can also be a direct blow to the tendon causing a rupture. There is typically a popping feeling or even a popping sound described during the occurance of the rupture. Typically there is pain with swelling in the region. Often the patient is unable to put weight on this foot as there is too much pain. Diagnosis If an Achilles tendon rupture is suspected, it is important to consult a doctor straight away so that an accurate diagnosis can be made and appropriate treatment recommended. Until a doctor can be consulted it is important to let the foot hang down with the toes pointed to the ground. This prevents the ends of the ruptured tendon pulling any farther apart. The doctor will take a full medical history, including any previous Achilles tendon injuries and what activity was being undertaken at the time the present injury occurred. The doctor will also conduct a physical examination and will check for swelling, tenderness and range of movement in the lower leg and foot. A noticeable gap may be able to be felt in the tendon at the site of the rupture. This is most obvious just after the rupture has occurred and swelling will eventually make this gap difficult to feel. One test commonly used to confirm an Achilles tendon rupture is the Thomson test. For this test the patient lies face down on an examination table. The doctor then squeezes the calf muscles; an action that would normally cause the foot to point like a ballerina (plantar flexion). When a partial rupture has occurred the foot's ability to point may be decreased. When a complete rupture has occurred, the foot may not point at all. Ultrasound scanning of the Achilles tendon may also be recommended in order to assist with the diagnosis. Non Surgical Treatment Once the Achilles tendon is partially damaged, one should exercise great care. The risk of rupture is high and if pain is associated with walking, one should consult with an orthopedic surgeon or a sports physician. A complete rupture of the Achilles tendon is never treated at home. It is important to understand that there are no minerals, nutrients, or herbs to treat Achilles tendon injury and any delay just worsens the recovery.  Surgical Treatment Surgery may be indicated directly following injury rather than conservative care. Repair of an achilles tendon rupture is greatly varied for each clinical situation. There may be a direct repair of the ends of the tendon with suture, or possibly a tendon graft used to augment the tendon. Post-operatively, the period of immobilization will depend on the size of the defect that was repaired and how it was completed. Usually the immobilization is between 6-10 weeks. This repair may allow for a complete return to normal function, but in many instances the healing is complicated with adhesions and a partial loss of range of motion. There may be a continued soft tissue defect noted and a permanent or prolonged swelling.
Surgical Treatment Surgery may be indicated directly following injury rather than conservative care. Repair of an achilles tendon rupture is greatly varied for each clinical situation. There may be a direct repair of the ends of the tendon with suture, or possibly a tendon graft used to augment the tendon. Post-operatively, the period of immobilization will depend on the size of the defect that was repaired and how it was completed. Usually the immobilization is between 6-10 weeks. This repair may allow for a complete return to normal function, but in many instances the healing is complicated with adhesions and a partial loss of range of motion. There may be a continued soft tissue defect noted and a permanent or prolonged swelling.
What Is Pes Planus?

?Life begins at 40,? goes an old quote, ?and so do fallen arches.? It?s time to toss that negative idea out the window and get the real facts on fallen arches and what you can do about them. We have all seen what our footprints look like as we walked across sand or left a water trail after getting out of the bathtub. The narrow part of the footprint is where your natural arch exists. What gives you that arch are tendons that pull together to create an upward curve. When your tendons are not properly pulling together, you start to lose that natural arch. This condition is known as flat foot or fallen arch.
Causes
Fallen arches can be the result of other conditions such as overuse, stretching or tearing of the posterior tibial tendon (which attaches to a bone in the foot and runs up the calf of the lower leg at a tension which pulls up the arch) which reduces its ability to maintain tension in the tendon. Whether or not the condition is caused by overpronation, this is the likely outcome for runners, whose arches are no longer strong enough to take the constant strain of bearing the body?s weight on impact, causing joint, postural and muscular problems.
Symptoms
Symptoms that should be checked by a pediatrician include foot pain, sores or pressure areas on the inner side of the foot, a stiff foot, limited side-to-side foot motion, or limited up-and-down ankle motion. For further treatment you should see a pediatric orthopedic surgeon or podiatrist experienced in childhood foot conditions.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
Non Surgical Treatment
The typical treatment for pain from fallen arches is an arch insert. While many people experience dramatic pain relief from this, others continue to suffer from chronic achy feet despite the arch support. The problem with this approach is that it does not do anything to strengthen the weak ligaments that may be at the root of the problem and, thus, does not alleviate the chronic pain that people with this condition experience. Another standard practice of modern medicine is to use steroids or to prescribe anti-inflammatory medications. However, in the long run, these treatments do more damage than good. Cortisone shots and anti-inflammatory drugs have been shown to produce short-term pain benefit, but both result in long-term loss of function and even more chronic pain by actually inhibiting the healing process of soft tissues and accelerating cartilage degeneration. Plus, long-term use of these drugs can lead to other sources of chronic pain, allergies and leaky gut syndrome.
Surgical Treatment

Surgical correction is dependent on the severity of symptoms and the stage of deformity. The goals of surgery are to create a more functional and stable foot. There are multiple procedures available to the surgeon and it may take several to correct a flatfoot deformity. Stage one deformities usually respond to conservative or non-surgical therapy such as anti-inflammatory medication, casting, functional orthotics or a foot ankle orthosis called a Richie Brace. If these modalities are unsuccessful surgery is warranted. Usually surgical treatment begins with removal of inflammatory tissue and repair of the posterior tibial tendon. A tendon transfer is performed if the posterior tibial muscle is weak or the tendon is badly damaged. The most commonly used tendon is the flexor digitorum longus tendon. This tendon flexes or moves the lesser toes downward. The flexor digitorum longus tendon is utilized due to its close proximity to the posterior tibial tendon and because there are minimal side effects with its loss. The remainder of the tendon is sutured to the flexor hallucis longus tendon that flexes the big toe so that little function is loss. Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
Achilles Tendonitis Recovery
 Achilles Tendinitis is the inflammation of the Achilles Tendon located in the heel, and is typically caused by overuse of the affected limb. Most often, it occurs in athletes who are not training with the proper techniques and/or equipment. When the Achilles Tendon is injured, blood vessels and nerve fibers from surrounding areas migrate into the tendon, and the nerve fibers may be responsible for the discomfort. Healing is often slow in this area due to the comparably low amount of cellular activity and blood flowing through the area.
Achilles Tendinitis is the inflammation of the Achilles Tendon located in the heel, and is typically caused by overuse of the affected limb. Most often, it occurs in athletes who are not training with the proper techniques and/or equipment. When the Achilles Tendon is injured, blood vessels and nerve fibers from surrounding areas migrate into the tendon, and the nerve fibers may be responsible for the discomfort. Healing is often slow in this area due to the comparably low amount of cellular activity and blood flowing through the area.
Causes
Possible factors leading to the development of Achilles tendonitis include the following. Implementing a new exercise regiment such as running uphill or climbing stairs. Change in exercise routine, boosting intensity or increasing duration. Shoes worn during exercise lack support, either because the soles are worn out or poor shoe design. Omitting proper warm-up prior to strenuous exercise. Running on a hard or uneven surface. Deformation in foot such as a flat arch, or any anatomic variation that puts unnecessary strain on the Achilles tendon.
Symptoms
Recurring localized pain, sometimes severe, along the tendon during or a few hours after running. Morning tenderness about an inch and a half above the point where the Achilles tendon is attached to the heel bone. Sluggishness in your leg. Mild or severe swelling. Stiffness that generally diminishes as the tendon warms up with use.
Diagnosis
Confirming Achilles tendonitis may involve imaging tests. X-rays provide images of the bones of the foot and leg. Magnetic resonance imaging (MRI) is useful for detecting ruptures and degeneration of tissue. Ultrasound shows tendon movement, related damage, and inflammation.
Nonsurgical Treatment
With proper care for the area, the pain in the tendon should lessen over three weeks, but it should be noted that the healing of the area continues and doesn't even peak until at least six weeks following the initial injury. This is due to scar tissue formation, which initially acts like the glue to bond the tissue back together. Scar tissue will continue to form past six weeks in some cases and as long as a year in severe cases. After 6 months this condition is considered chronic and much more difficult to treat. The initial approach to treating Achilles tendonitis is to support and protect the tendons by bracing any areas of the tendon that are being pulled on during use. It is important to loosen up the tendon, lessen the pain, and minimize any inflammation.

Surgical Treatment
Mini-Open Achilles Tendon Repair. During a mini-open Achilles tendon repair surgery, 2 to 8 small stab incisions are made to pull the edges of the tendon tear together and suture the torn edges to repair the damage. During this procedure the surgeon will make one 3 to 4 cm long incision on the back of your ankle and 2 to 4 smaller vertical incisions around the long incision. These smaller veritical incisions are made with a pair of surgical scissors and are commonly referred to as "stab incisions". Once the incisions are opened up, the surgeon will place precise sutures with non-absorbable stitches to strengthen the damaged Achilles tendon tissue. This suturing technique reduces the amount of scar tissue on the tendon after surgery and provides better surface healing of the skin. Unlike the traditional method of an open surgery, this procedure has less risks and complications involved. To learn about all risks you may face be sure to speak to your doctor.
Prevention
Maintaining strength and flexibility in the muscles of the calf will help reduce the risk of tendinitis. Overusing a weak or tight Achilles tendon makes you more likely to develop tendinitis.
Working With Fallen Arches

The appearance of flat feet is normal and common in infants, partly due to "baby fat" which masks the developing arch and partly because the arch has not yet fully developed. The human arch develops in infancy and early childhood as part of normal muscle, tendon, ligament and bone growth. Training of the feet, especially by foot gymnastics and going barefoot on varying terrain, can facilitate the formation of arches during childhood, with a developed arch occurring for most by the age of four to six years. Flat arches in children usually become proper arches and high arches while the child progresses through adolescence and into adulthood. A survey of 297 suburban school children up to the age of 10 years at Allahabad in U.P. in India revealed 40.32% children under 5 years, 22.15% children between 5-10 years and 15.48% children above 10 years but below 15 years having bilateral flat foot.
Causes
As children grow, their legs will experience developmental changes that can result in excess flattening of the arches with weight bearing. One example is genu valgum, or knock-knees, a usually normal, temporary condition in children at different stages of growth. A tight calf muscle or Achilles tendon can also contribute to a flat foot. Many children will experience tight calf muscles as they go through growth spurts. Conditions that are present at birth and are often diagnosed early include: metatarsus adductus, calcaneovalgus and congenital vertical talus. Tarsal coalitions are congenitally fused foot bones that cause a rigid flat foot often associated with painful muscle spasms. This type of flat foot is usually diagnosed later in childhood or in adulthood. Any condition that causes loose ligaments can result in a flat foot or lower-than-normal arch. Ligaments are bands of tissue that connect bones to each other and have an important role in giving form to foot arches. An example of a condition that causes loosening of ligaments is pregnancy, where normal hormonal changes relax the ligaments. Diseases that cause loose ligaments include Ehlers-Danlos syndrome, Marfan's syndrome and rheumatoid arthritis. If one leg is longer than the other, one foot may be flat in relation to the other to compensate. Usually the foot on the longer limb will have a flatter arch in an effort to shorten that limb, balancing-out the unevenness. Leg length inequality can be caused by spinal abnormalities such as scoliosis. It can also be due to an actual difference in length of one leg bone compared to the other.
Symptoms
Fallen arches symptoms may include the following. Being unable to slip fingers underneath arches. Inwards rolling of foot and ankle when running. Knee problems due to lack of support from feet.
Diagnosis
An examination of the foot is enough for the health care provider to diagnose flat foot. However, the cause must be determined. If an arch develops when the patient stands on his or her toes, the flat foot is called flexible and no treatment or further work-up is necessary. If there is pain associated with the foot or if the arch does not develop with toe-standing, x-rays are necessary. If a tarsal coalition is suspected, a CT scan is often ordered. If a posterior tibial tendon injury is suspected, your health care provider may recommend an MRI.
Non Surgical Treatment
When pain results from a fallen arch, the physician may prescribe these. Rest and ice. A brace to help support the fallen arch. Physical therapy to strengthen and stretch the foot. Orthotics (arch supports) to compensate for a fallen arch. The physician may tell the patient to choose shoes that have proper arch supports and avoid non-supportive shoes such as flip-flops. If obesity contributed to the fallen arch, the patient should lose weight.
Surgical Treatment

A better approach is to strengthen the weakened ligaments with Prolotherapy, supplemented by an arch support if the condition has existed for several years. Chronic pain is most commonly due to tendon and ligament weakness, or cartilage deterioration. The safest and most effective natural medicine treatment for repairing tendon, ligament and cartilage damage is Prolotherapy. In simple terms, Prolotherapy stimulates the body to repair painful areas. It does so by inducing a mild inflammatory reaction in the weakened ligaments and cartilage. Since the body heals by inflammation, Prolotherapy stimulates healing. Prolotherapy offers the most curative results in treating chronic pain. It effectively eliminates pain because it attacks the source: the fibro-osseous junction, an area rich in sensory nerves. What?s more, the tissue strengthening and pain relief stimulated by Prolotherapy is permanent.
Prevention
Wear Supportive Footwear. Spend the money it takes to get proper fitting and quality footwear with good arch supports. Most sufferers of fallen arches and plantar fasciitis are born with high arches that sag as they get older. Good footwear can prevent this from becoming a problem. Flat feet, however, can become just as problematic. So, really we should all be wearing good footwear to avoid this potentially painful condition. Take It Easy. If your heel starts to hurt, take a rest. If the pain doesn?t go away after several days of resting, it may be time to see a podiatrist. Orthotics. Special insoles to support the arch of the foot can provide some much needed help. You can buy these at your local drugstore (not recommended), or you can have them specially made and custom fit for your feet. It can take awhile to get just the right one for your foot, but sometimes it can be just what you needed. Weight Control. Yes, maintaining a sensible diet with your ideal weight can be beneficial in many ways. It makes sense to think that the more weight your arches are supporting, the more easily they will fall and become painful.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
What Can Cause Arch Pain ?
If you are dealing with chronic pain in the arch of your foot (the area between the ball and heel) it may be diagnosed as arch strain. While there are several potential causes for arch pain, the most common cause is plantar fasciitis. The plantar fascia is the band of ligaments that runs along the sole of the foot, connecting the heel bone to the metatarsals (bones just behind the toes.) Its job is to support the arch of your foot, and to put some ?spring in your step.? But, unfortunately, it?s the sight of an all-to-common inflammation that causes intense pain in the heel and across the bottom of the foot. This inflammation and pain is known as plantar fasciitis.

Causes
Recent research has found a link with changes to the tendon in the foot and an increase in a type of protein called proteolytic enzyme. These enzymes can break down some areas of the tendon, weakening it and causing the foot arch to fall. Similar changes are also seen in other conditions, such as Achilles tendonitis. This could have important implications for treating flat feet because medication that specifically targets these enzymes could provide an alternative to surgery. However, further research is needed and this type of treatment is thought to be about 10 to 15 years away.
Symptoms
Persistant pain and selling under the ball of the foot and extending towards the toes (most commonly the 2nd). Some swelling may be disable on the top of the foot along with redness. Often a sensation of 'walking on the bones for the foot' will be described, and there is a positive Lachman's test. Often a tear will result in the toes splaying (daylight sign) and clawing.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
Non Surgical Treatment
This is a common foot condition that can be easily treated. If you suffer from arch pain avoid high-heeled shoes whenever possible. Try to choose footwear with a reasonable heel, soft leather uppers, shock absorbing soles and removable foot insoles. When the arch pain is pronation related (flat feet), an orthotic designed with a medial heel post and proper arch support is recommended for treating the pain. This type of orthotic will control over-pronation, support the arch and provide the necessary relief. If the problem persists, consult your foot doctor.

Surgical Treatment
In rare cases, surgery may be needed if a child has flat feet caused by a problem they're born with (a congenital abnormality). The foot may need to be straightened or the bones may need to be separated if they're fused together. Painkillers and insoles are the first treatment options for flat feet that are caused by a joint problem, such as arthritis or a torn tendon. However, surgery may be recommended if the injury or condition is severely affecting your feet. Where flat feet are caused by a condition that affects the nervous system, special shoes, insoles, or supportive foot or leg braces may be needed. Again, in severe cases, an operation may be needed to straighten the feet.
Prevention
Strap the arches into the anatomically correct positions with athletic tape and leave them like this for some time. If the fallen arches are an issue with the muscular structure, this may give the muscles an opportunity to strengthen. This is definitely not a fallen arches cure all the time but it can help prevent it more times than not. Ask a doctor or physical therapists to show you how to do this taping. Find shoes that fit. This may require that you get your foot measured and molded to ensure that the shoe will fit. Shoes that are too big, too tight or too short, may not directly cause the fallen arches, but they can assist with the damage to the area. These shoes should have thick cushioning inside and have plenty of room for your toes. Walk without shoes as much as possible. Shoes directly assist with weakening and distorting the arches of the feet so going without shoes can actually help strengthen your arches and prevent fallen arches. Walking on hard and bumpy surfaces barefooted makes the muscles in your feet strengthen in order to prevent injury. It is a coping mechanism by your body. Insert heel cups or insoles into the shoes that you wear the most. Many people wear uncomfortable shoes to work and these are the same shoes that cause their arches the most problems. Inserting the heel cups and insoles into these shoes can prevent fallen arches from occurring. Many people place these inserts into all their shoes to ensure support. Ask a medical professional, either your doctor or a physical therapist, about daily foot exercises that may keep the arches stronger than normal. Many times, you can find exercises and stretches on the Internet on various websites. Curling your toes tightly and rotating your feet will help strengthen your longitudinal arches. Relax your feet and shake them for a minute or so before you do any arch exercises. This will loosen the muscles in your feet that stay tight due to normal daily activities. Wear rigid soled sandals whenever possible to provide a strong support for your arches. Wooden soled sandals are the best ones if available. Walk or jog on concrete as much as you can. This will create a sturdy support for your arches. Running or walking in sandy areas or even on a treadmill, does not give rigid support. Instead, these surfaces absorb the step, offering no support for arches.
Stretching Exercises
Start in an L-Sit position. (If you?re hips and hamstrings are tight sit up on a box or phone book to be able to achieve a tall back position. You can even sit on a box with your back supported against a wall!) Keeping the legs straight, but not locked, reach both heels out away from your body to ?Flex? the ankles. Try to avoid pulling back with the toes to flex. Keep the toes relaxed and lead from the heel to hinge the foot into the flexed position. Hold the flexed foot and breathe. Take 3-5 breaths and see if you can reach farther through the heel to deepen the flex on each exhale. To transition to the pointed position, begin by pointing the foot to move the ankles as far as possible in the other direction. Once the ankles have reached their endpoint, use the muscles along the sole of the foot to point the toes. Inhale to continue lengthening out through the top of the foot, exhale to deepen the contraction under the sole of the foot to point the toes. Take 3-5 breaths. Then release the toes, and begin reaching out through the heel to hinge the ankle into the flexed position to repeat the exercise. Continue to flex and the point for 5-10 repetitions.
Pain In The Foot's Arch What Are The Reasons ?
Pain or strain in your foot arches is a common sports injury and often linked to inflammation of the plantar fascia, the shock absorption ligament along the bottom of each foot. The pain can also highlight underlying issues to do with the structure of your arches.
Causes
The arches are the primary structures of the body that absorb and return force to and from the body to the outside world when we are on our feet. When something happens to these structures, pain and injury may result. There can be many causes of arch pain. Direct force trauma, ligament sprains, muscle strains, poor biomechanical alignment,stress fractures, overuse, inflammatory arthritis or the tightness or lack of tightness of the joints in the foot may all cause pain in the arch. Injury to the plantar fascia is a common cause of arch pain. The plantar fascia is the thick, connective tissue which supports the arch on the bottom of the foot. It runs from the calcaneus (heel) forwards to the heads of the metatarsals. When the plantar fascia is damaged, the resulting inflammatory response may become a source of arch pain.
Symptoms
The primary symptom is pain or aching in the arch area. This can be accompanied by inflammation and tenderness. If the pain is caused by the plantar fascia, it is likely to be considerably more severe in the mornings due to the muscles being unused. If you notice that the twinges of pain you have are most commonly associated with or immediately after exercise, you might want to visit a good athletic shoe store to make sure you are wearing the right kind of shoe. Another cause of arch pain is plantar fasciitis. The plantar fascia is a tough tissue structure that holds the bottom part of the arch in place. The fascia often becomes inflamed and sore, usually as a result of repetitive motion (for example, very common in those who stand on their feet for work). The pain is often noticeable first thing in the morning and worse with activity.
Diagnosis
After you describe your symptoms and discuss your concerns, your doctor will examine your foot. Your doctor will look for these signs. A high arch. An area of maximum tenderness on the bottom of your foot, just in front of your heel bone. Pain that gets worse when you flex your foot and the doctor pushes on the plantar fascia. The pain improves when you point your toes down. Limited "up" motion of your ankle.
Non Surgical Treatment
Anti-inflammatory medications such as ibuprofen and aspirin can provide short-term relief from foot pain associated with fallen arches, notes the American Academy of Orthopaedic Surgeons. Doctors sometimes inject the foot with a corticosteroid medication, which acts as an anti-inflammatory, to relieve acute pain. Although medications can provide symptom relief, they do not correct the underlying foot abnormality.

Surgical Treatment
In rare cases, surgery may be needed if a child has flat feet caused by a problem they're born with (a congenital abnormality). The foot may need to be straightened or the bones may need to be separated if they're fused together. Painkillers and insoles are the first treatment options for flat feet that are caused by a joint problem, such as arthritis or a torn tendon. However, surgery may be recommended if the injury or condition is severely affecting your feet. Where flat feet are caused by a condition that affects the nervous system, special shoes, insoles, or supportive foot or leg braces may be needed. Again, in severe cases, an operation may be needed to straighten the feet.
Stretching Exercises
Massage therapy is a great way to loosen muscles and help improve mobility in in your feet. As many people with foot pain have discovered, tight muscles in your legs or back can lead to tense foot muscles. All those muscles are connected, so tension in your back can cause tension in your legs which can pull the tendons in your feet and cause stiffness and pain. Getting acupuncture or a professional full body massage are probably the best ways to deal with this, but there are also some simple tricks you can do at home to help keep muscles limber. These are great for loosening up and improving circulation, both before and after exercise. Place a tennis ball under the arch of your bare foot and roll it around, stretching the muscles in your foot and promoting blood flow. You can also roll the ball under your calves and upper legs to work out stiffness and knots. If you feel the tennis ball is too easy, try a lacrosse ball for deeper massaging. This is also demonstrated in the exercise video above. Use a foam roller, those big overpriced rolls of foam that are now available in every department and sporting goods store are fantastic for self-massage (why a roll of foam costs $30 is beyond us, but they do work wonders-our advice is to not waste money on the more expensive fancy grooved ones because even the simplest rollers work great). The exercises you can do with foam rollers seem to be endless, and there are literally hundreds of free videos online showing how to use them to massage every part of your body. Here's one we picked out that specifically targets foot and leg muscles related to arches and plantar fasciitis.